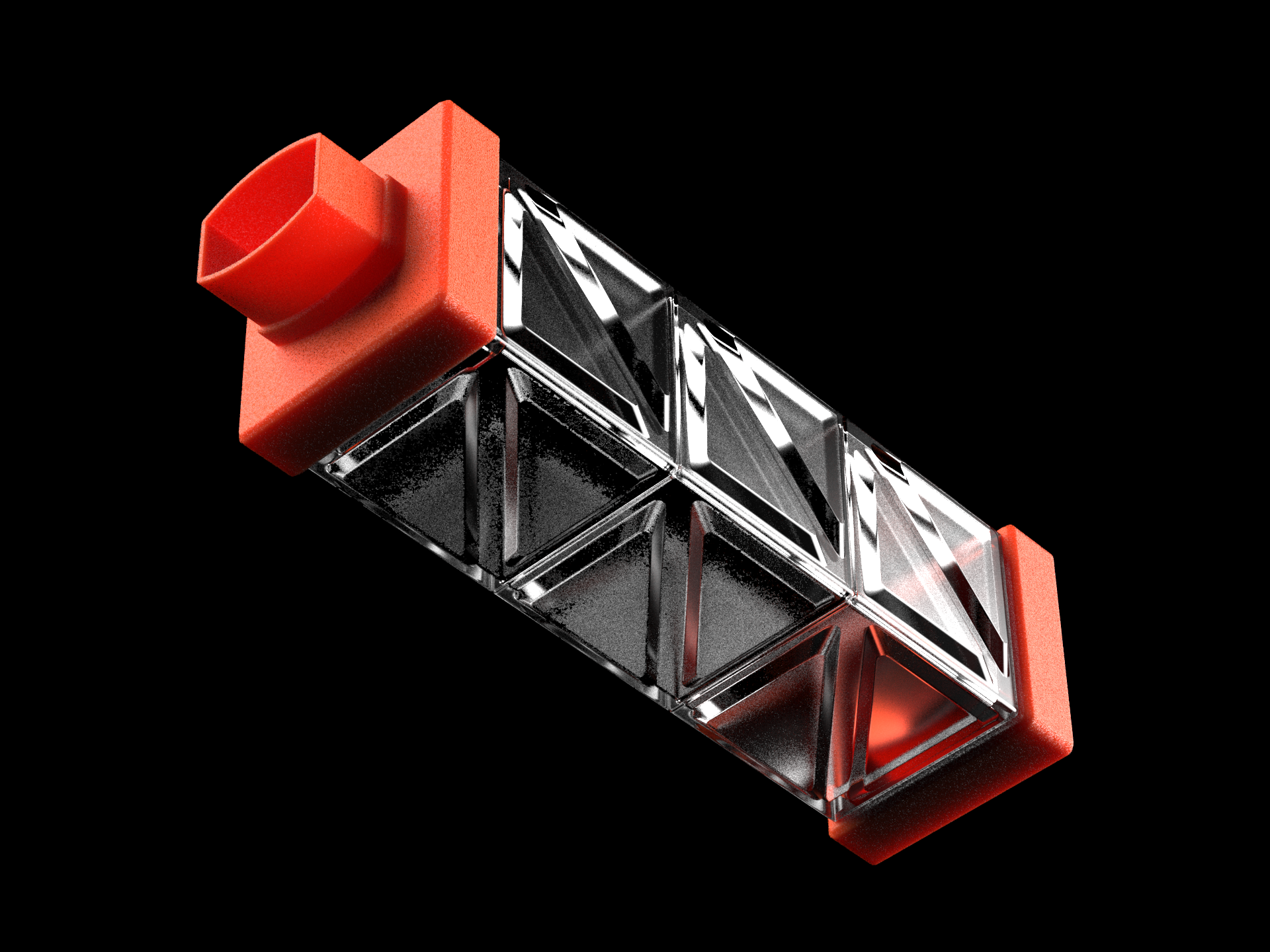
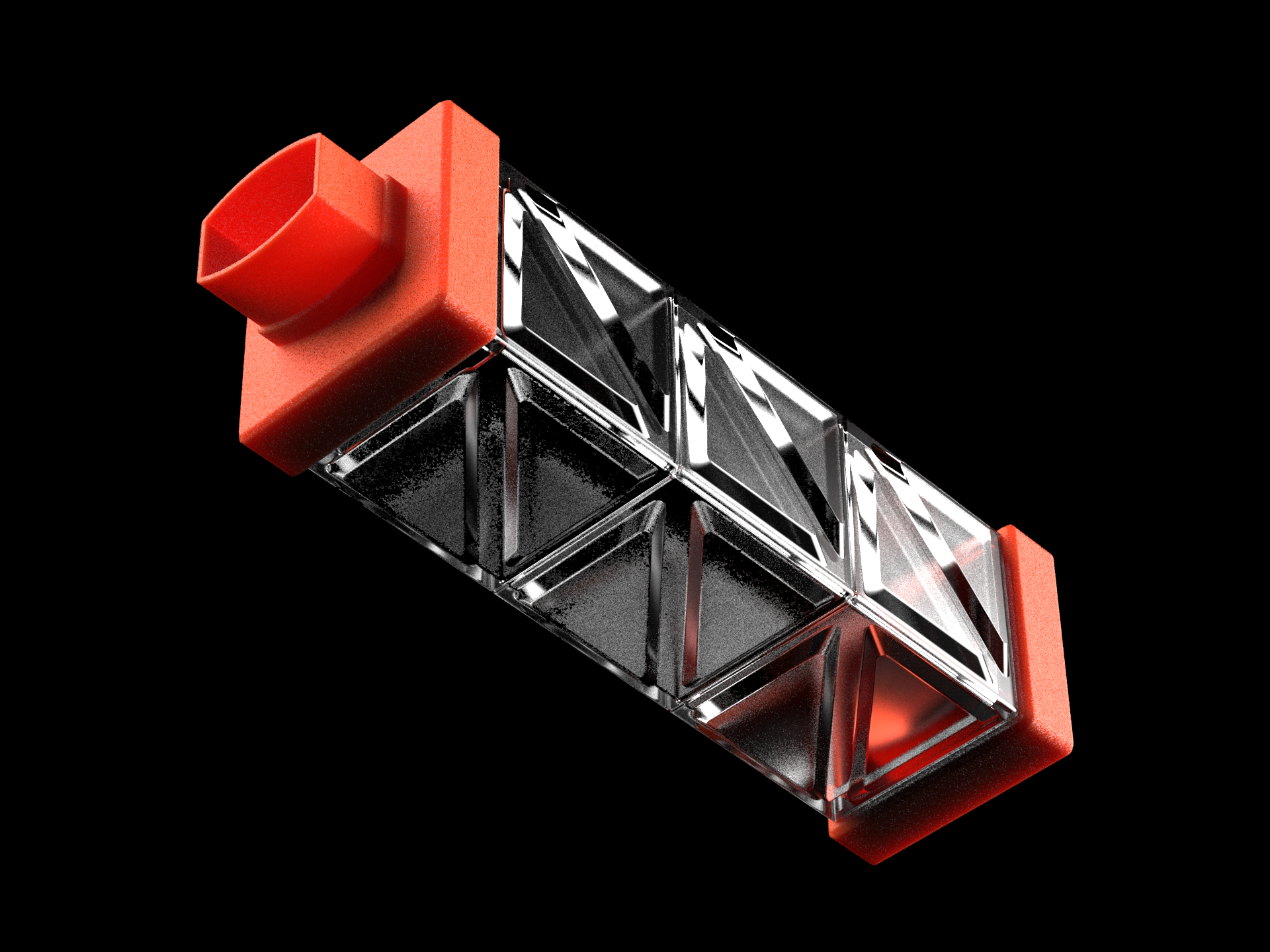
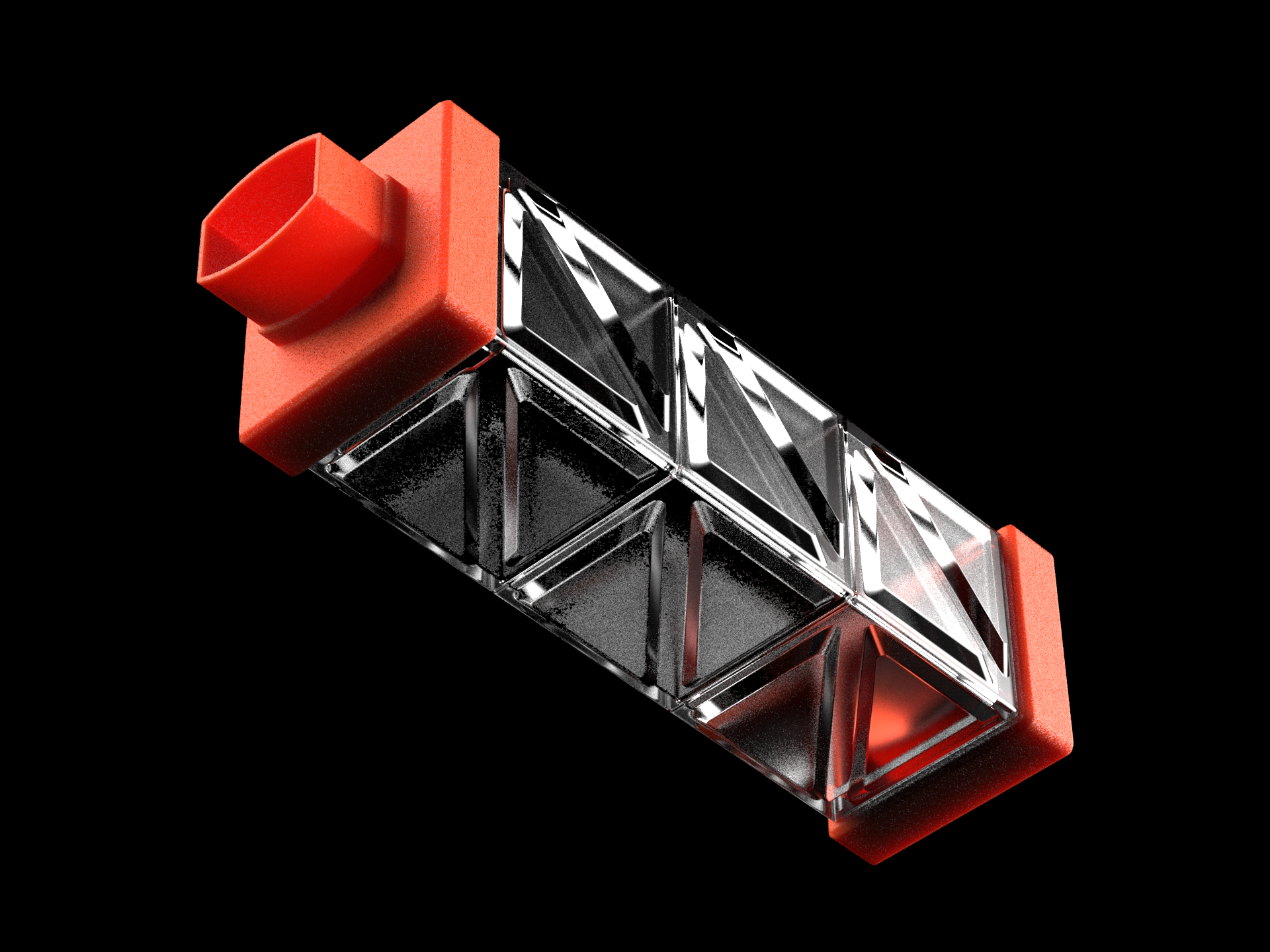
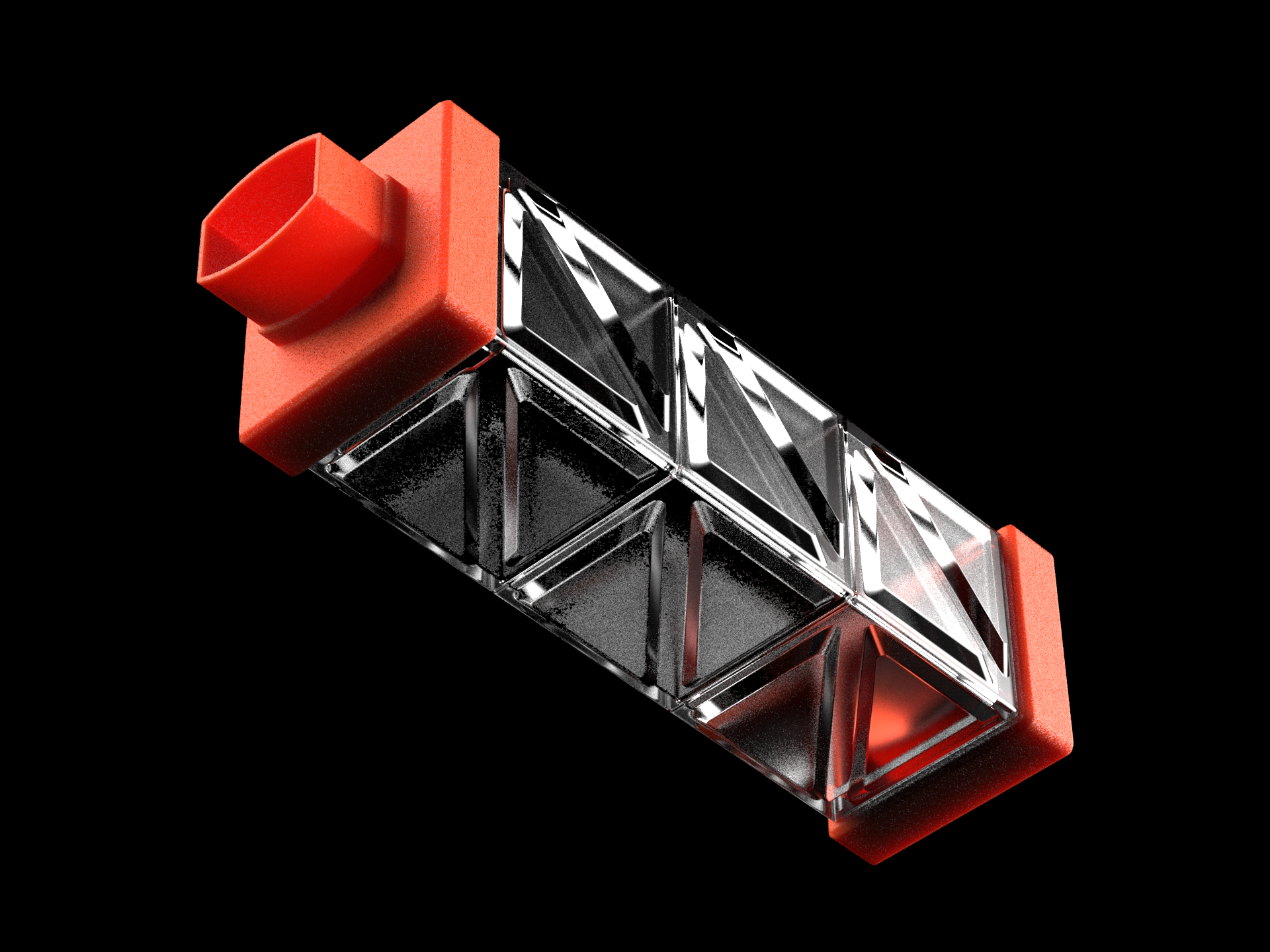
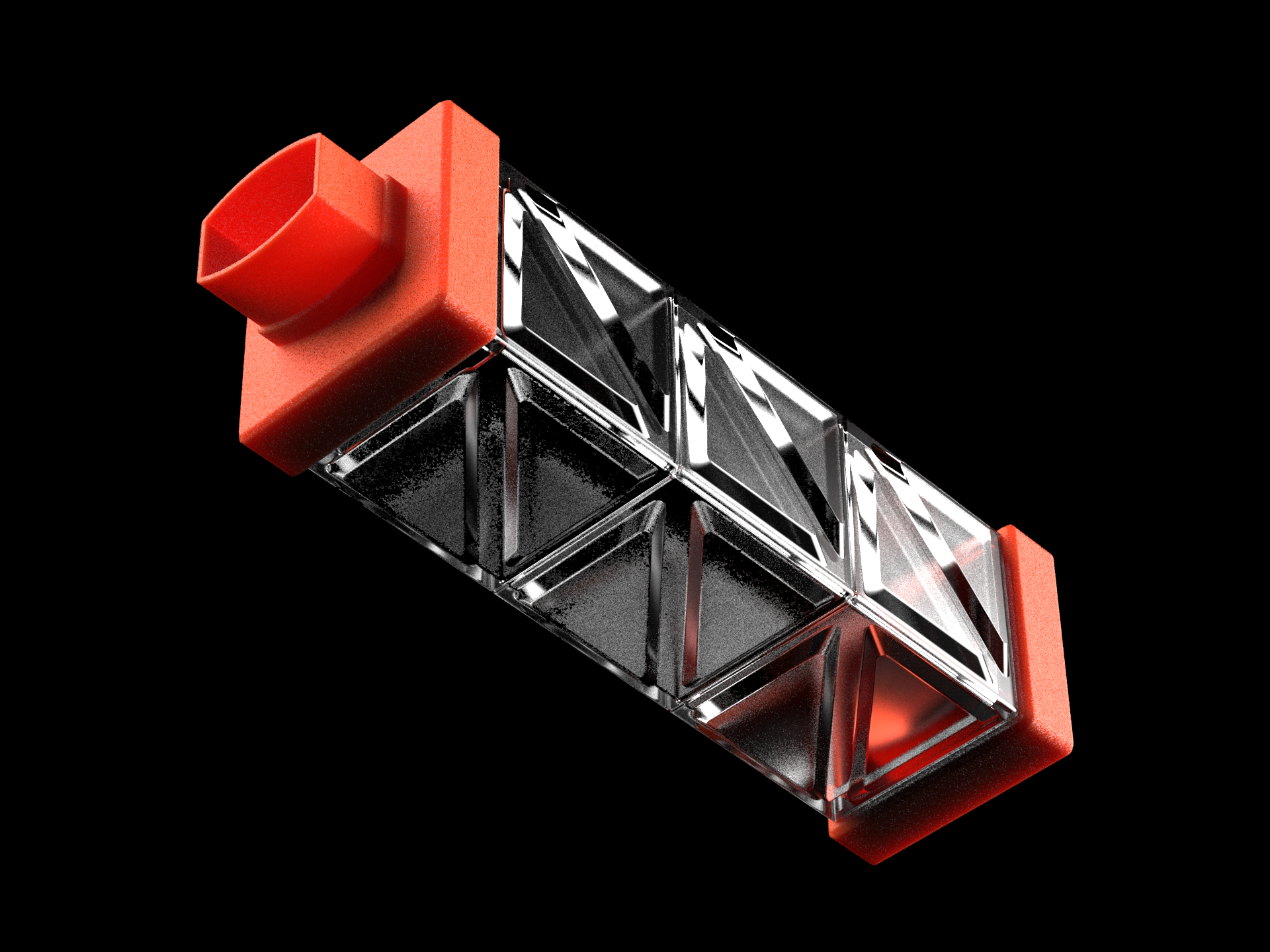
Respira is a collapsible asthma spacer concept designed to make inhaler use more practical and effective. Traditional spacers, though crucial for improving drug delivery, are often bulky and inconvenient, leading to low adoption despite proven benefits. Inspired by origami, Respira’s foldable design combines portability with optimal airflow. This project details agile prototyping to create a user-friendly solution.
context
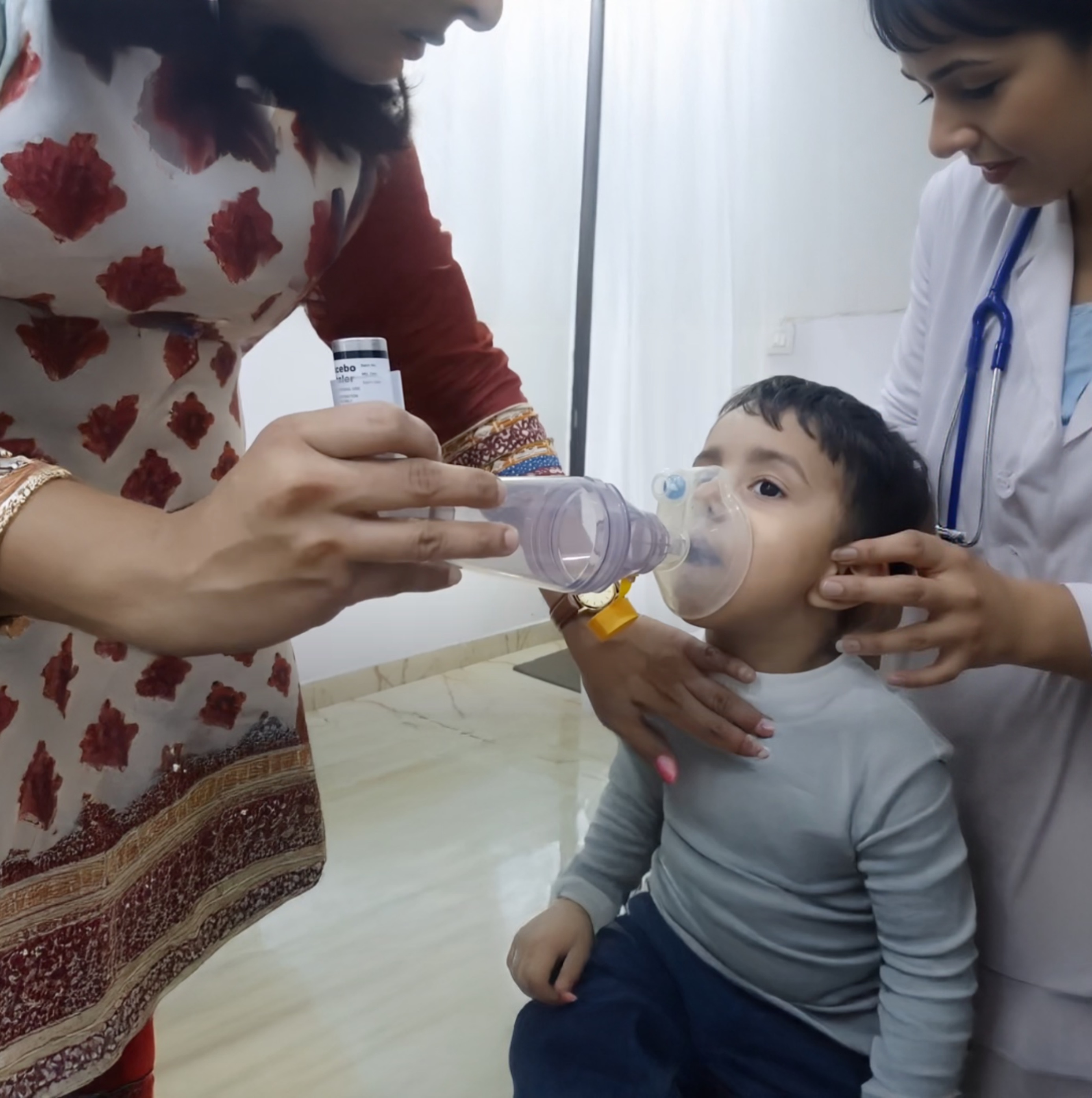
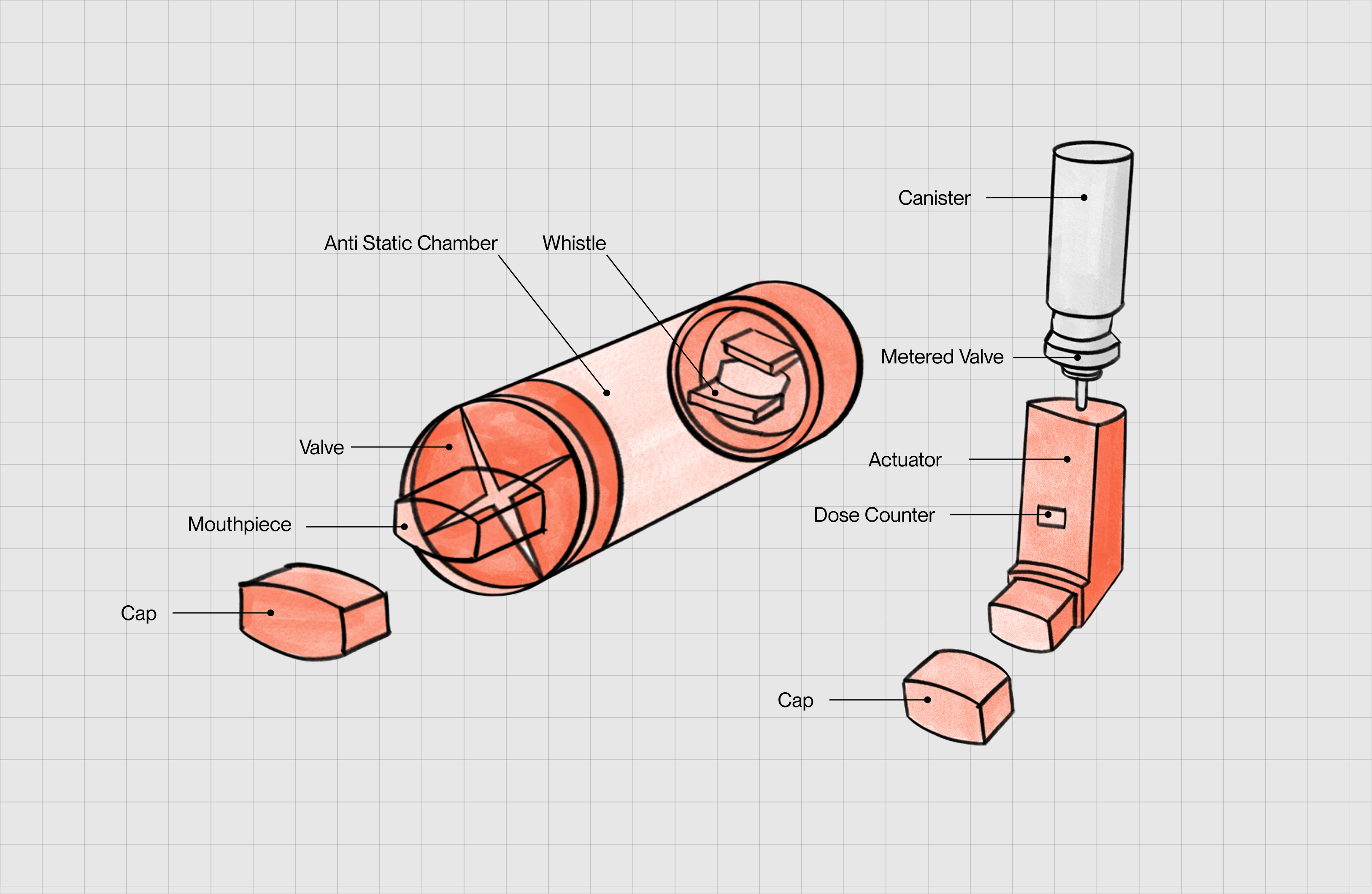
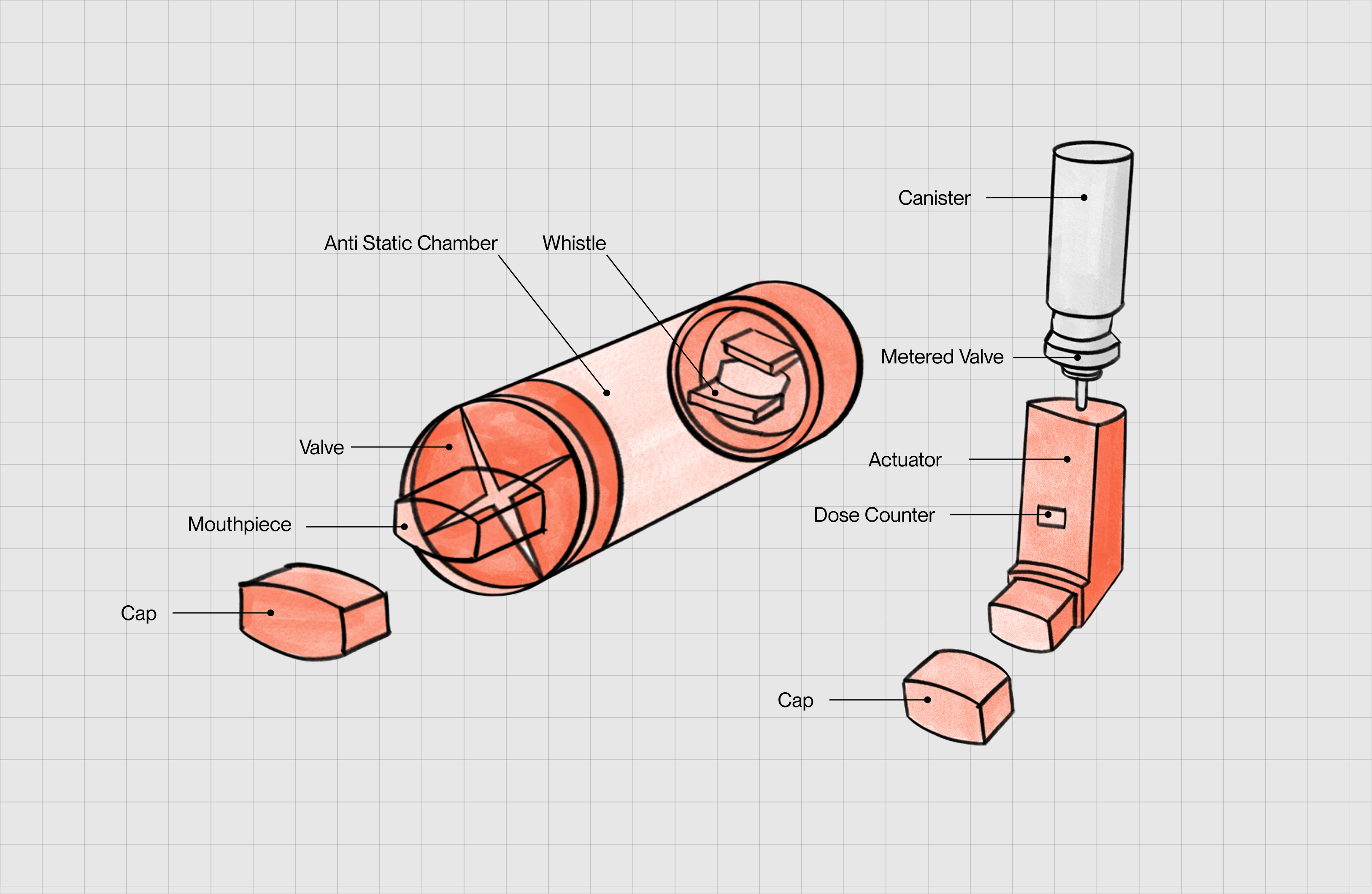
Asthma affects over 300 million people worldwide, and that number continues to rise, especially in urban environments where pollution, lifestyle, and stress compound the risk. For most patients, metered-dose inhalers (MDIs) are the frontline tools for managing symptoms, delivering bronchodilators or corticosteroids directly to the lungs. But despite their clinical importance, inhalers are only as effective as the way they’re used.
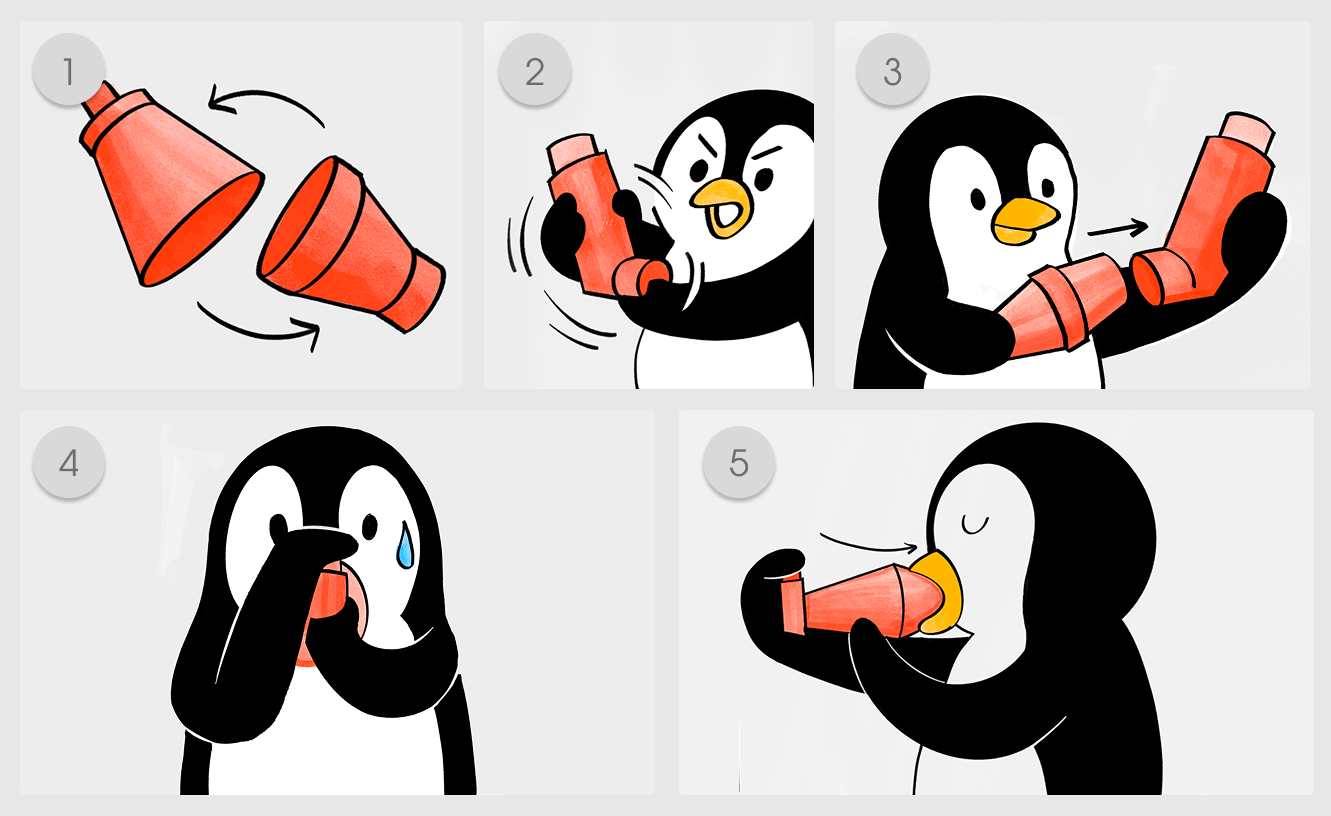
Here's the catch: using an MDI correctly requires a surprising level of coordination, pressing down on the canister and inhaling at just the right moment. Most people, especially children, the elderly, or those in distress, struggle with this. As a result, up to 90% of the medication can end up in the mouth or throat instead of the lungs, leading to poor symptom control and unnecessary side effects like oral thrush and hoarseness.
To solve this, spacers were introduced, tube-like attachments that hold the medication in a chamber, giving users time to inhale slowly and deeply. They work. In fact, studies show that spacers significantly improve medication delivery to the lungs and reduce complications. So, why don’t more people use them? and how can we design a spacer that can be more widely used? This is the problem we set out to solve in this project.








Process
Secondary research
To better understand the nuances of this problem, we began with secondary research, exploring the broader landscape of respiratory illnesses, inhaler systems, and spacer technologies currently in use.
We reviewed MDIs, DPIs, SMIs, and nebulizers and intentionally centered our work on the spacer + MDI ecosystem because that’s where coordination burden and real-world misuse are most visible. We captured how actuation timing, inspiratory flow demands, and user coaching influence deposition, then tied those to the everyday life of an Indian user who needs a discreet, pocketable solution.
We ran a mini pricing and availability scan to understand what a typical Indian patient encounters at pharmacies. That work surfaced a pragmatic constraint set: limited affordability bands, highly variable counseling quality, and inconsistent access to higher-end antistatic VHCs. These realities shaped guardrails for materials, manufacturing paths, and maintenance rituals.
We traced the evolution of spacers from early holding chambers to kid-oriented motivators and paper fold-outs. The pattern was consistent: attempts at portability often sacrificed airtightness, stable internal volume, antistatic behavior, or cleaning ease. That history told us not to “make it smaller,” but to redesign the architecture so portability and performance reinforce each other.
Secondary research
To better understand the nuances of this problem, we began with secondary research, exploring the broader landscape of respiratory illnesses, inhaler systems, and spacer technologies currently in use.
We reviewed MDIs, DPIs, SMIs, and nebulizers and intentionally centered our work on the spacer + MDI ecosystem because that’s where coordination burden and real-world misuse are most visible. We captured how actuation timing, inspiratory flow demands, and user coaching influence deposition, then tied those to the everyday life of an Indian user who needs a discreet, pocketable solution.
We ran a mini pricing and availability scan to understand what a typical Indian patient encounters at pharmacies. That work surfaced a pragmatic constraint set: limited affordability bands, highly variable counseling quality, and inconsistent access to higher-end antistatic VHCs. These realities shaped guardrails for materials, manufacturing paths, and maintenance rituals.
We traced the evolution of spacers from early holding chambers to kid-oriented motivators and paper fold-outs. The pattern was consistent: attempts at portability often sacrificed airtightness, stable internal volume, antistatic behavior, or cleaning ease. That history told us not to “make it smaller,” but to redesign the architecture so portability and performance reinforce each other.
Secondary research
To better understand the nuances of this problem, we began with secondary research, exploring the broader landscape of respiratory illnesses, inhaler systems, and spacer technologies currently in use.
We reviewed MDIs, DPIs, SMIs, and nebulizers and intentionally centered our work on the spacer + MDI ecosystem because that’s where coordination burden and real-world misuse are most visible. We captured how actuation timing, inspiratory flow demands, and user coaching influence deposition, then tied those to the everyday life of an Indian user who needs a discreet, pocketable solution.
We ran a mini pricing and availability scan to understand what a typical Indian patient encounters at pharmacies. That work surfaced a pragmatic constraint set: limited affordability bands, highly variable counseling quality, and inconsistent access to higher-end antistatic VHCs. These realities shaped guardrails for materials, manufacturing paths, and maintenance rituals.
We traced the evolution of spacers from early holding chambers to kid-oriented motivators and paper fold-outs. The pattern was consistent: attempts at portability often sacrificed airtightness, stable internal volume, antistatic behavior, or cleaning ease. That history told us not to “make it smaller,” but to redesign the architecture so portability and performance reinforce each other.


Primary research
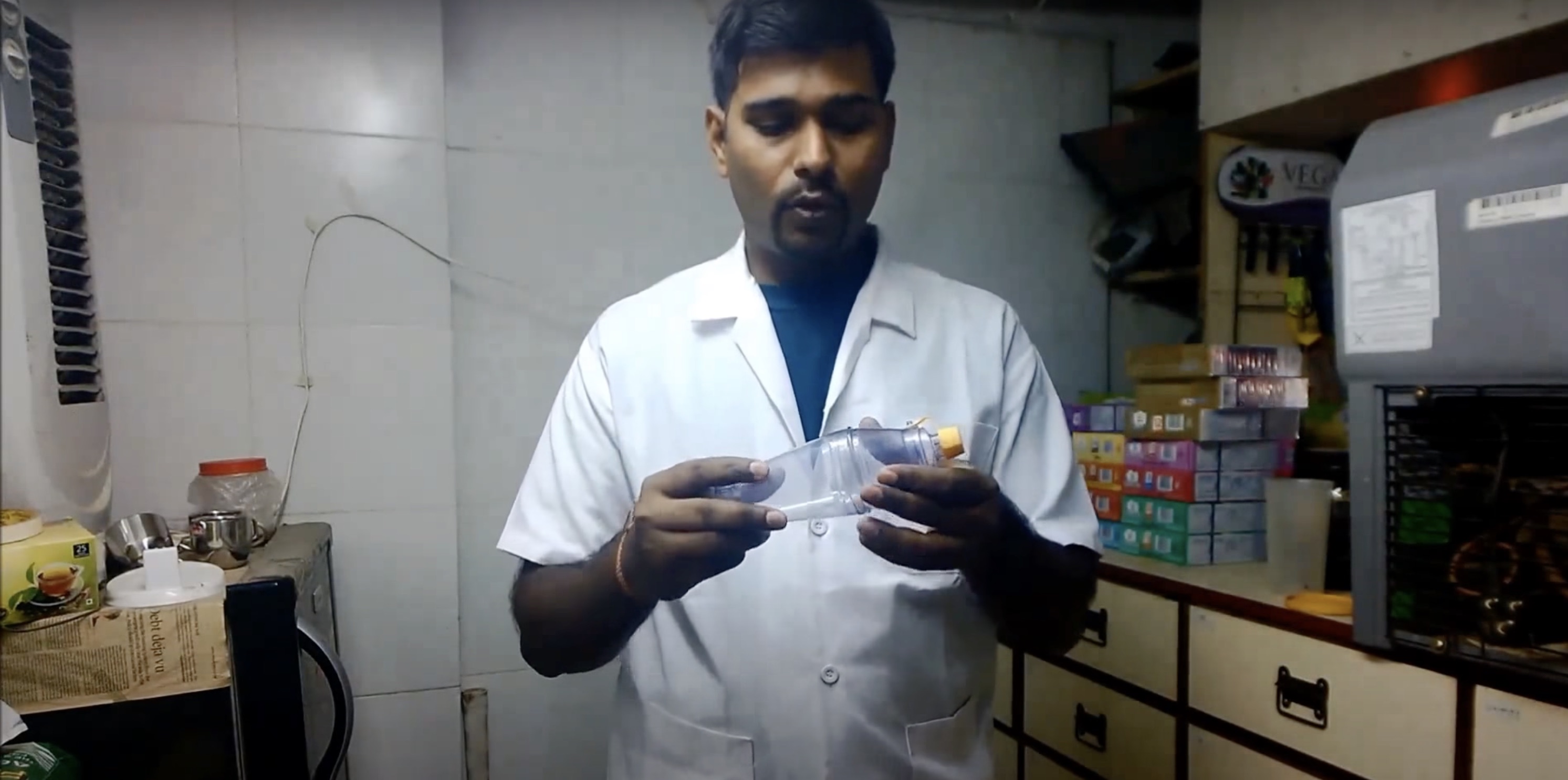
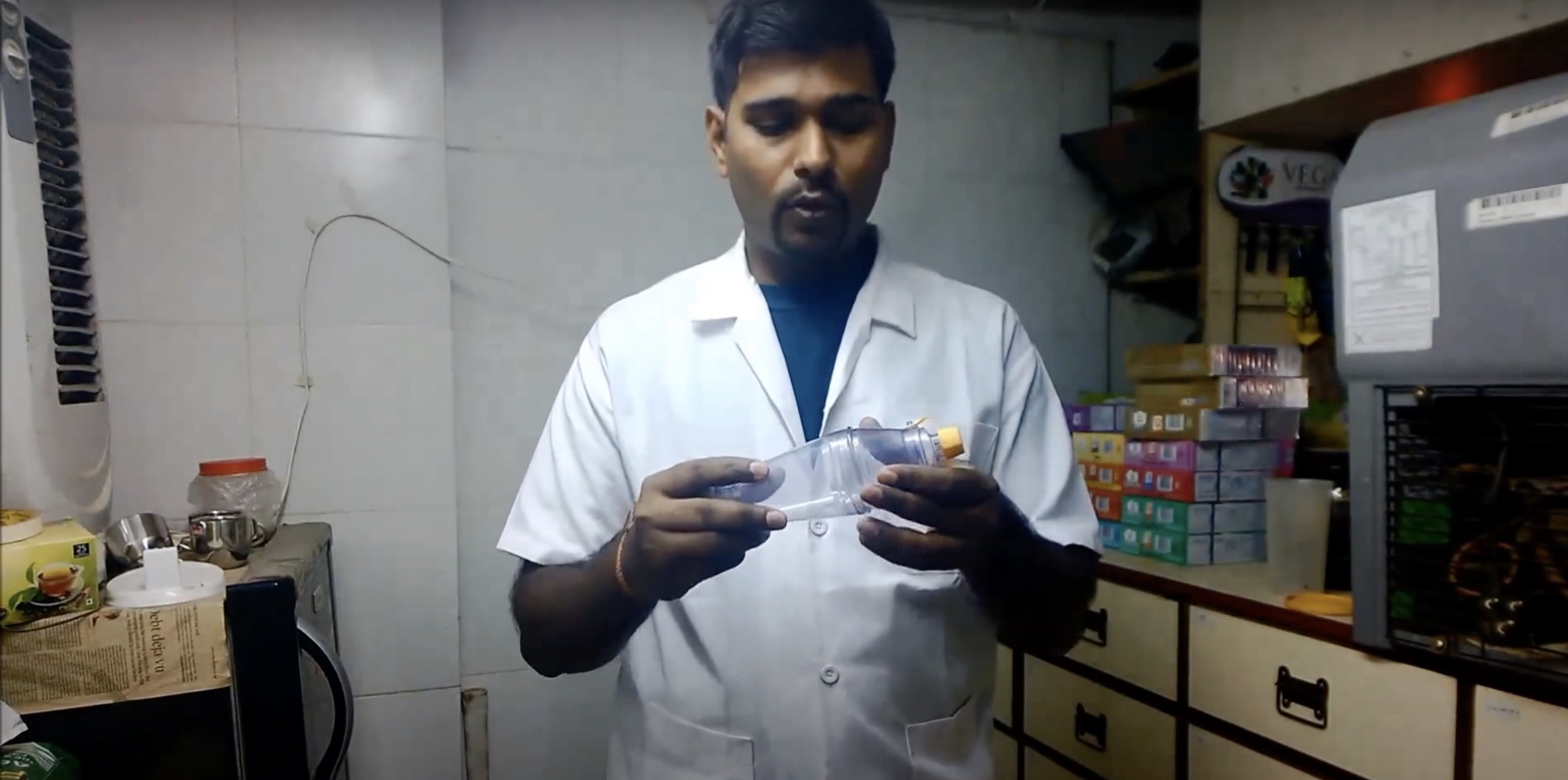
We adopted a fast, opportunistic fieldwork cadence to put lived experience above assumptions. We spoke with patients and clinicians, watched technique instruction in the wild, and handled devices alongside users. The intent was to let real barriers direct the brief.
Stakeholder touchpoints included chats with GPs, a pulmonologist, a school nurse, pharmacy staff, caregivers, and patients in Ahmedabad. We observed not just what people said, but how they learned and performed the technique under time pressure. Recurrent frictions emerged quickly: social stigma around using a bulky attachment in public, unclear “why” behind the spacer, and the cognitive overhead of carrying a second object.
We wrote out correct technique in plain language and compared it with what we saw. Even when users owned a spacer, inconsistent instruction meant poor habits, multiple puffs per inhale, rushed breathing, or skipping the device entirely. That reframed our challenge as a behavior + communication problem as much as an industrial-design one.
To prioritize criteria, we used lightweight probes, co-handling existing spacers, semi-structured questioning, and simple sorting of “what matters most right now.” A striking signal was how often embarrassment and pocketability ranked above abstract performance gains. That insight pushed us to pursue mechanisms that deploy confidently with one hand and look discreet enough to use anywhere.





Primary research
We adopted a fast, opportunistic fieldwork cadence to put lived experience above assumptions. We spoke with patients and clinicians, watched technique instruction in the wild, and handled devices alongside users. The intent was to let real barriers direct the brief.
Stakeholder touchpoints included chats with GPs, a pulmonologist, a school nurse, pharmacy staff, caregivers, and patients in Ahmedabad. We observed not just what people said, but how they learned and performed the technique under time pressure. Recurrent frictions emerged quickly: social stigma around using a bulky attachment in public, unclear “why” behind the spacer, and the cognitive overhead of carrying a second object.
We wrote out correct technique in plain language and compared it with what we saw. Even when users owned a spacer, inconsistent instruction meant poor habits, multiple puffs per inhale, rushed breathing, or skipping the device entirely. That reframed our challenge as a behavior + communication problem as much as an industrial-design one.
To prioritize criteria, we used lightweight probes, co-handling existing spacers, semi-structured questioning, and simple sorting of “what matters most right now.” A striking signal was how often embarrassment and pocketability ranked above abstract performance gains. That insight pushed us to pursue mechanisms that deploy confidently with one hand and look discreet enough to use anywhere.
Primary research
We adopted a fast, opportunistic fieldwork cadence to put lived experience above assumptions. We spoke with patients and clinicians, watched technique instruction in the wild, and handled devices alongside users. The intent was to let real barriers direct the brief.
Stakeholder touchpoints included chats with GPs, a pulmonologist, a school nurse, pharmacy staff, caregivers, and patients in Ahmedabad. We observed not just what people said, but how they learned and performed the technique under time pressure. Recurrent frictions emerged quickly: social stigma around using a bulky attachment in public, unclear “why” behind the spacer, and the cognitive overhead of carrying a second object.
We wrote out correct technique in plain language and compared it with what we saw. Even when users owned a spacer, inconsistent instruction meant poor habits, multiple puffs per inhale, rushed breathing, or skipping the device entirely. That reframed our challenge as a behavior + communication problem as much as an industrial-design one.
To prioritize criteria, we used lightweight probes, co-handling existing spacers, semi-structured questioning, and simple sorting of “what matters most right now.” A striking signal was how often embarrassment and pocketability ranked above abstract performance gains. That insight pushed us to pursue mechanisms that deploy confidently with one hand and look discreet enough to use anywhere.
Primary research
We adopted a fast, opportunistic fieldwork cadence to put lived experience above assumptions. We spoke with patients and clinicians, watched technique instruction in the wild, and handled devices alongside users. The intent was to let real barriers direct the brief.
Stakeholder touchpoints included chats with GPs, a pulmonologist, a school nurse, pharmacy staff, caregivers, and patients in Ahmedabad. We observed not just what people said, but how they learned and performed the technique under time pressure. Recurrent frictions emerged quickly: social stigma around using a bulky attachment in public, unclear “why” behind the spacer, and the cognitive overhead of carrying a second object.
We wrote out correct technique in plain language and compared it with what we saw. Even when users owned a spacer, inconsistent instruction meant poor habits, multiple puffs per inhale, rushed breathing, or skipping the device entirely. That reframed our challenge as a behavior + communication problem as much as an industrial-design one.
To prioritize criteria, we used lightweight probes, co-handling existing spacers, semi-structured questioning, and simple sorting of “what matters most right now.” A striking signal was how often embarrassment and pocketability ranked above abstract performance gains. That insight pushed us to pursue mechanisms that deploy confidently with one hand and look discreet enough to use anywhere.






Problem reframing
Why do people not use the spacer?
From observations, interviews, and affinity mapping, four themes kept repeating: portability pain, public stigma, unclear benefits, and low clinical emphasis. In short, spacers often fit medical guidelines better than they fit real life.
Existing evidence echoes this reality. Usage remains low: only ~20–30% of pediatric emergency departments use MDIs with spacers over nebulizers, and one survey reported just 21% of Canadian physicians recommending spacers for wheezing children. Even when owned, many users skip them due to bulk, cleaning hassle, embarrassment, or vague instructions.
Outcomes research is mixed—some studies show little long-term advantage when medication is already optimized, so clinicians may under-prioritize spacers. Yet when education is solid, both spacer use and inhaler technique improve. The barrier isn’t whether spacers “work,” but whether they’re easy, accessible, and appealing enough to use every day.
Final brief: How might we redesign asthma spacers to be more portable, intuitive, and discreet — without compromising on drug delivery effectiveness?
Problem reframing
Why do people not use the spacer?
From observations, interviews, and affinity mapping, four themes kept repeating: portability pain, public stigma, unclear benefits, and low clinical emphasis. In short, spacers often fit medical guidelines better than they fit real life.
Existing evidence echoes this reality. Usage remains low: only ~20–30% of pediatric emergency departments use MDIs with spacers over nebulizers, and one survey reported just 21% of Canadian physicians recommending spacers for wheezing children. Even when owned, many users skip them due to bulk, cleaning hassle, embarrassment, or vague instructions.
Outcomes research is mixed—some studies show little long-term advantage when medication is already optimized, so clinicians may under-prioritize spacers. Yet when education is solid, both spacer use and inhaler technique improve. The barrier isn’t whether spacers “work,” but whether they’re easy, accessible, and appealing enough to use every day.
Final brief: How might we redesign asthma spacers to be more portable, intuitive, and discreet — without compromising on drug delivery effectiveness?
Problem reframing
Why do people not use the spacer?
From observations, interviews, and affinity mapping, four themes kept repeating: portability pain, public stigma, unclear benefits, and low clinical emphasis. In short, spacers often fit medical guidelines better than they fit real life.
Existing evidence echoes this reality. Usage remains low: only ~20–30% of pediatric emergency departments use MDIs with spacers over nebulizers, and one survey reported just 21% of Canadian physicians recommending spacers for wheezing children. Even when owned, many users skip them due to bulk, cleaning hassle, embarrassment, or vague instructions.
Outcomes research is mixed—some studies show little long-term advantage when medication is already optimized, so clinicians may under-prioritize spacers. Yet when education is solid, both spacer use and inhaler technique improve. The barrier isn’t whether spacers “work,” but whether they’re easy, accessible, and appealing enough to use every day.
Final brief: How might we redesign asthma spacers to be more portable, intuitive, and discreet — without compromising on drug delivery effectiveness?
Problem reframing
Why do people not use the spacer?
From observations, interviews, and affinity mapping, four themes kept repeating: portability pain, public stigma, unclear benefits, and low clinical emphasis. In short, spacers often fit medical guidelines better than they fit real life.
Existing evidence echoes this reality. Usage remains low: only ~20–30% of pediatric emergency departments use MDIs with spacers over nebulizers, and one survey reported just 21% of Canadian physicians recommending spacers for wheezing children. Even when owned, many users skip them due to bulk, cleaning hassle, embarrassment, or vague instructions.
Outcomes research is mixed—some studies show little long-term advantage when medication is already optimized, so clinicians may under-prioritize spacers. Yet when education is solid, both spacer use and inhaler technique improve. The barrier isn’t whether spacers “work,” but whether they’re easy, accessible, and appealing enough to use every day.
Final brief: How might we redesign asthma spacers to be more portable, intuitive, and discreet — without compromising on drug delivery effectiveness?

Agile prototyping (Form factor)
Brief 1 : Make spacers more compact
We explored origami-inspired structures not as a visual trope but as a way to reconcile portability with a stable internal chamber. We screened fold families for even expansion, structural stability, and clean airflow paths. We built, tried, and discarded aggressively to learn fast.
We evaluated Miura folds, wave geometries, square accordions, and twisting cuboids. Square accordion behaved like camera bellows and gave us predictable axial expansion. Twisting cuboids offered an intuitive “rotate-to-deploy” mental model, while some wave patterns achieved near-flat pocket profiles but risked internal cornering that could trap aerosol.
We moved quickly from paper to laminate and coated fiber sheets to test fold memory, seam alignment, and durability through repeated cycles. The goal was a chamber that stays flat in the pocket yet feels rigid and trustworthy when deployed.
To get beyond “looks aerodynamic,” we ran a DIY aerosol visualization inside prototypes to reveal dead zones, turbulence pockets, and deposition hot spots. That simple test killed pretty forms that sabotaged delivery, and it validated bellows-like geometries that kept flowlines clean.
Agile prototyping (Form factor)
Brief 1 : Make spacers more compact
We explored origami-inspired structures not as a visual trope but as a way to reconcile portability with a stable internal chamber. We screened fold families for even expansion, structural stability, and clean airflow paths. We built, tried, and discarded aggressively to learn fast.
We evaluated Miura folds, wave geometries, square accordions, and twisting cuboids. Square accordion behaved like camera bellows and gave us predictable axial expansion. Twisting cuboids offered an intuitive “rotate-to-deploy” mental model, while some wave patterns achieved near-flat pocket profiles but risked internal cornering that could trap aerosol.
We moved quickly from paper to laminate and coated fiber sheets to test fold memory, seam alignment, and durability through repeated cycles. The goal was a chamber that stays flat in the pocket yet feels rigid and trustworthy when deployed.
To get beyond “looks aerodynamic,” we ran a DIY aerosol visualization inside prototypes to reveal dead zones, turbulence pockets, and deposition hot spots. That simple test killed pretty forms that sabotaged delivery, and it validated bellows-like geometries that kept flowlines clean.
Agile prototyping (Form factor)
Brief 1 : Make spacers more compact
We explored origami-inspired structures not as a visual trope but as a way to reconcile portability with a stable internal chamber. We screened fold families for even expansion, structural stability, and clean airflow paths. We built, tried, and discarded aggressively to learn fast.
We evaluated Miura folds, wave geometries, square accordions, and twisting cuboids. Square accordion behaved like camera bellows and gave us predictable axial expansion. Twisting cuboids offered an intuitive “rotate-to-deploy” mental model, while some wave patterns achieved near-flat pocket profiles but risked internal cornering that could trap aerosol.
We moved quickly from paper to laminate and coated fiber sheets to test fold memory, seam alignment, and durability through repeated cycles. The goal was a chamber that stays flat in the pocket yet feels rigid and trustworthy when deployed.
To get beyond “looks aerodynamic,” we ran a DIY aerosol visualization inside prototypes to reveal dead zones, turbulence pockets, and deposition hot spots. That simple test killed pretty forms that sabotaged delivery, and it validated bellows-like geometries that kept flowlines clean.

Agile prototyping (Interactions)
Brief 2 : Enhance the user experience
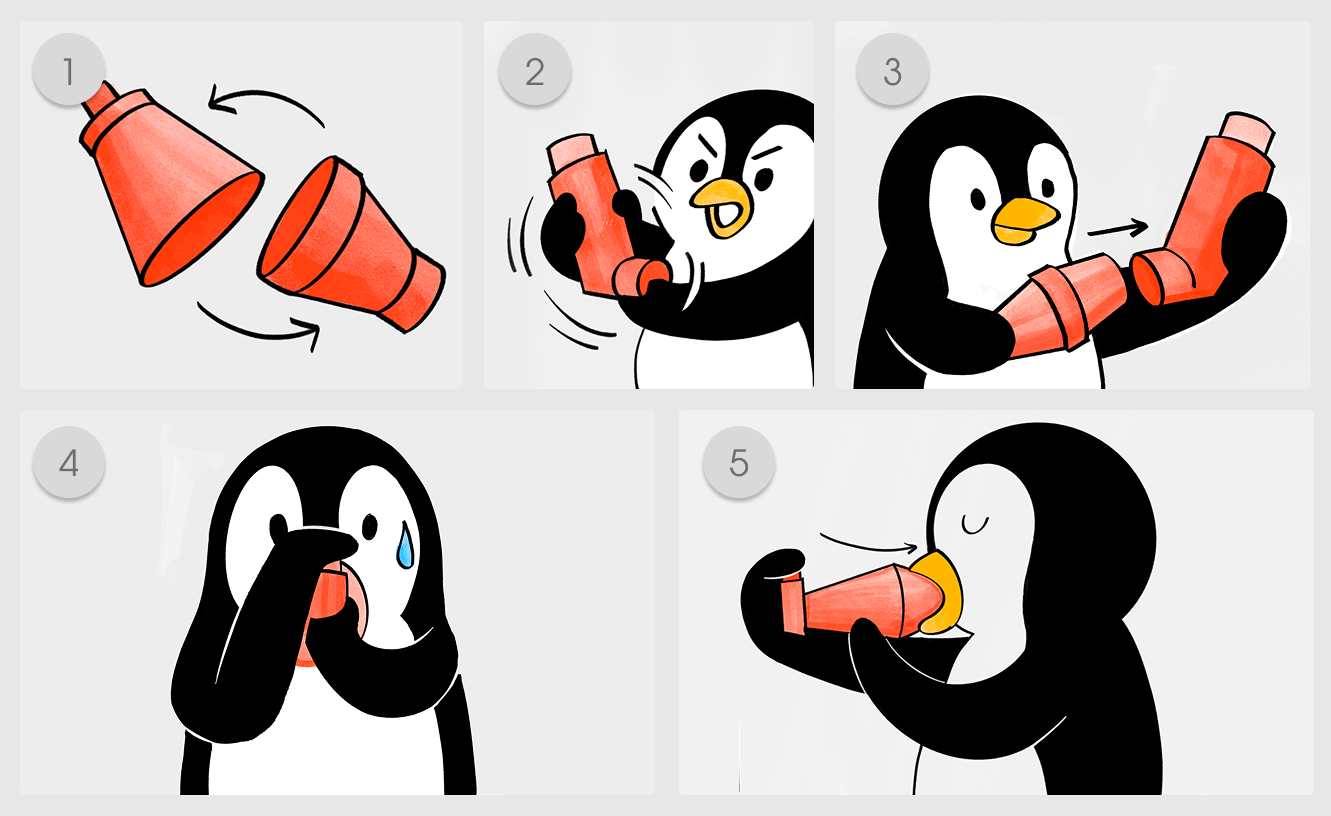
We treated deployment as a stress-state interaction: one hand free, shallow breath, maybe in public. We prototyped mechanisms that make “ready” obvious and failure unlikely. We pared the motion down to a single confident action with tactile or visual confirmation.
We tried a sliding drawer-stack expansion that feels like opening a compact, a clamshell hinge with a distinct tactile lock, and a balloon-style inflation concept that prioritized comfort at the mouth but lacked internal rigidity. We measured perceived faff: how long users hesitated, how often they double-checked, and whether they trusted the seal.
We also explored inhaler-integrated variants to remove the “two objects” cognitive load. Clip-in or stow-in approaches improved carry behavior but introduced tolerancing and cleaning tradeoffs, so we documented those carefully for future engineering passes.
Across iterations, we timed setup, watched grip security, and stress-tested the MDI connection while users simulated hurry. Designs that communicated “locked and ready” without words consistently outperformed technically similar forms that required a second look.
.gif)

Agile prototyping (Interactions)
Brief 2 : Enhance the user experience
We treated deployment as a stress-state interaction: one hand free, shallow breath, maybe in public. We prototyped mechanisms that make “ready” obvious and failure unlikely. We pared the motion down to a single confident action with tactile or visual confirmation.
We tried a sliding drawer-stack expansion that feels like opening a compact, a clamshell hinge with a distinct tactile lock, and a balloon-style inflation concept that prioritized comfort at the mouth but lacked internal rigidity. We measured perceived faff: how long users hesitated, how often they double-checked, and whether they trusted the seal.
We also explored inhaler-integrated variants to remove the “two objects” cognitive load. Clip-in or stow-in approaches improved carry behavior but introduced tolerancing and cleaning tradeoffs, so we documented those carefully for future engineering passes.
Across iterations, we timed setup, watched grip security, and stress-tested the MDI connection while users simulated hurry. Designs that communicated “locked and ready” without words consistently outperformed technically similar forms that required a second look.
Agile prototyping (Interactions)
Brief 2 : Enhance the user experience
We treated deployment as a stress-state interaction: one hand free, shallow breath, maybe in public. We prototyped mechanisms that make “ready” obvious and failure unlikely. We pared the motion down to a single confident action with tactile or visual confirmation.
We tried a sliding drawer-stack expansion that feels like opening a compact, a clamshell hinge with a distinct tactile lock, and a balloon-style inflation concept that prioritized comfort at the mouth but lacked internal rigidity. We measured perceived faff: how long users hesitated, how often they double-checked, and whether they trusted the seal.
We also explored inhaler-integrated variants to remove the “two objects” cognitive load. Clip-in or stow-in approaches improved carry behavior but introduced tolerancing and cleaning tradeoffs, so we documented those carefully for future engineering passes.
Across iterations, we timed setup, watched grip security, and stress-tested the MDI connection while users simulated hurry. Designs that communicated “locked and ready” without words consistently outperformed technically similar forms that required a second look.
Agile prototyping (Interactions)
Brief 2 : Enhance the user experience
We treated deployment as a stress-state interaction: one hand free, shallow breath, maybe in public. We prototyped mechanisms that make “ready” obvious and failure unlikely. We pared the motion down to a single confident action with tactile or visual confirmation.
We tried a sliding drawer-stack expansion that feels like opening a compact, a clamshell hinge with a distinct tactile lock, and a balloon-style inflation concept that prioritized comfort at the mouth but lacked internal rigidity. We measured perceived faff: how long users hesitated, how often they double-checked, and whether they trusted the seal.
We also explored inhaler-integrated variants to remove the “two objects” cognitive load. Clip-in or stow-in approaches improved carry behavior but introduced tolerancing and cleaning tradeoffs, so we documented those carefully for future engineering passes.
Across iterations, we timed setup, watched grip security, and stress-tested the MDI connection while users simulated hurry. Designs that communicated “locked and ready” without words consistently outperformed technically similar forms that required a second look.
.gif)




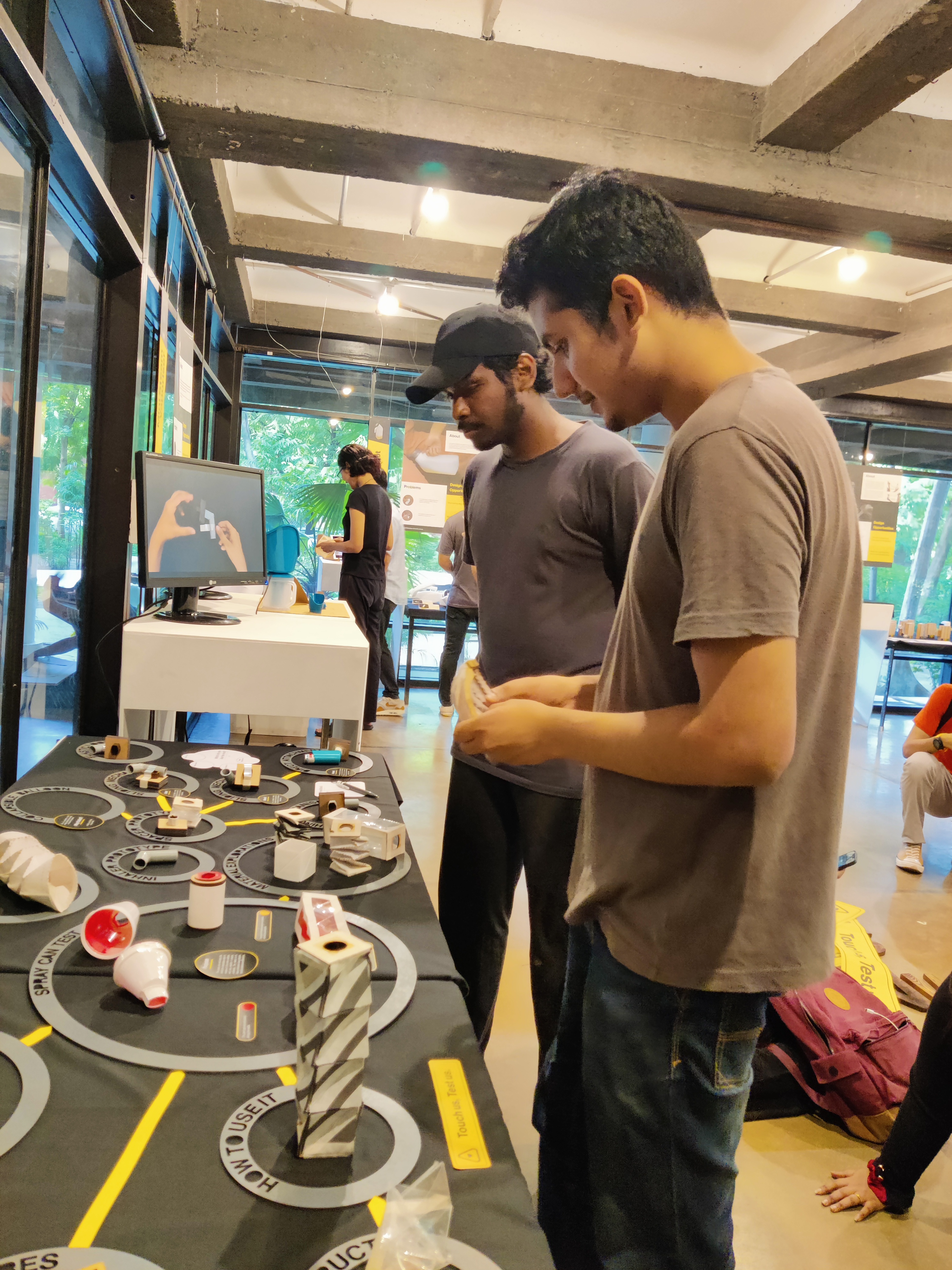
Final Outcome
We converged on an origami-inspired, pocket-friendly spacer architecture that deploys in one hand and preserves a clear airway. Exhibiting prototypes surfaced validation on portability and clarity and sharpened our next steps. We left with a direction, not just a model.
Feedback from users, designers and healthcare professionals emphasized the value of a crisp ready state and a mouth interface that feels familiar. Several people noted they would actually carry this in a pocket or small bag, which is where previous designs often lost the battle.
The process reinforced that agile make–test–learn reveals pitfalls paper logic misses. Dead zones, clumsy locks and material creep appeared only in hands-on cycles. That rhythm, rather than heavy up-front theorizing, moved the concept toward something people would actually use.
We defined next milestones around validated antistatic materials, refined airflow modeling, valve selection and small pilot trials to quantify deposition and time-to-effective-dose in real contexts.

Final Outcome
We converged on an origami-inspired, pocket-friendly spacer architecture that deploys in one hand and preserves a clear airway. Exhibiting prototypes surfaced validation on portability and clarity and sharpened our next steps. We left with a direction, not just a model.
Feedback from users, designers and healthcare professionals emphasized the value of a crisp ready state and a mouth interface that feels familiar. Several people noted they would actually carry this in a pocket or small bag, which is where previous designs often lost the battle.
The process reinforced that agile make–test–learn reveals pitfalls paper logic misses. Dead zones, clumsy locks and material creep appeared only in hands-on cycles. That rhythm, rather than heavy up-front theorizing, moved the concept toward something people would actually use.
We defined next milestones around validated antistatic materials, refined airflow modeling, valve selection and small pilot trials to quantify deposition and time-to-effective-dose in real contexts.

Final Outcome
We converged on an origami-inspired, pocket-friendly spacer architecture that deploys in one hand and preserves a clear airway. Exhibiting prototypes surfaced validation on portability and clarity and sharpened our next steps. We left with a direction, not just a model.
Feedback from users, designers and healthcare professionals emphasized the value of a crisp ready state and a mouth interface that feels familiar. Several people noted they would actually carry this in a pocket or small bag, which is where previous designs often lost the battle.
The process reinforced that agile make–test–learn reveals pitfalls paper logic misses. Dead zones, clumsy locks and material creep appeared only in hands-on cycles. That rhythm, rather than heavy up-front theorizing, moved the concept toward something people would actually use.
We defined next milestones around validated antistatic materials, refined airflow modeling, valve selection and small pilot trials to quantify deposition and time-to-effective-dose in real contexts.

Final Outcome
We converged on an origami-inspired, pocket-friendly spacer architecture that deploys in one hand and preserves a clear airway. Exhibiting prototypes surfaced validation on portability and clarity and sharpened our next steps. We left with a direction, not just a model.
Feedback from users, designers and healthcare professionals emphasized the value of a crisp ready state and a mouth interface that feels familiar. Several people noted they would actually carry this in a pocket or small bag, which is where previous designs often lost the battle.
The process reinforced that agile make–test–learn reveals pitfalls paper logic misses. Dead zones, clumsy locks and material creep appeared only in hands-on cycles. That rhythm, rather than heavy up-front theorizing, moved the concept toward something people would actually use.
We defined next milestones around validated antistatic materials, refined airflow modeling, valve selection and small pilot trials to quantify deposition and time-to-effective-dose in real contexts.





.jpg)